1 Introduction
In 2020, the World Health Organization (WHO) and United Nations described the surge of information, misinformation, and disinformation related to the COVID-19 virus as an “infodemic” [Zarocostas, 2020]. The following year, the United States (US) Surgeon General issued an official advisory warning the public about the urgent threat of health misinformation [Office of the Surgeon General, 2021]. Scientific misinformation has been conceptualized as “publicly available information that is misleading or deceptive relative to the best available scientific evidence or expertise at the time and that counters statements by actors or institutions who adhere to scientific principles without adding accurate evidence for consideration” [Southwell, Brennen, Paquin, Boudewyns & Zeng, 2022]. More specifically, health misinformation “can be defined as a health related claim of fact that is currently false due to a lack of scientific evidence” [Chou, Oh & Klein, 2018, p. 1].1
While the concept of health misinformation is not new [Thompson, Parrott & Nussbaum, 2011], an infodemic brings additional challenges as it presents an overabundance of information, accurate or not, hindering access to trustworthy sources and guidance [Tangcharoensathien et al., 2020; Zarocostas, 2020]. A glance at social media activity reveals why this label was justified: in March 2020, there were 550 million tweets posted to Twitter (now “X”) that included the terms coronavirus, corona virus, covid19, covid-19, covid_19, or pandemic [Pan American Health Organization, 2020]. Amid this health crisis, rising rates of vaccine rejection or hesitancy, even in areas with historically high levels of acceptance, were among the most worrying effects of this (mis)information overwhelm [Argote et al., 2021; Sallam, 2021].
As trusted members of society [Suran & Bucher, 2024], physicians and health organizations were called upon to combat the COVID-19 infodemic by leveraging technology and social media platforms to disseminate accurate health information to the public [Office of the Surgeon General, 2021]. Physicians answered this call [Topf & Williams, 2021], organizing to collectively use social media to amplify accurate medical information about the pandemic [Royan et al., 2022]. For example, the #ThisIsOurShot campaign, a grassroots digital coalition of “healthcare heroes” (doctors, nurses, pharmacists, and medical students), sought to provide accurate health information, promote effective health policy, and build trust in vaccines in particular and in science in general [ThisIsOurShot, n.d.]. Similarly, the Dear Pandemic project brought together researchers and clinicians to support women in navigating COVID-19 challenges, by sharing evidence-based information on social media in an effort to address pandemic misinformation and help their audience make informed health decisions [Those Nerdy Girls, 2022].
However, there is limited information about how and why physicians have used social media to share health information during the pandemic and whether their behavior will persist into the future. Thus, this study seeks to understand physicians’ experiences of using social media, specifically Twitter/X, to share health information during the COVID-19 context. We aim to describe physicians’ online communication practices and identify any shifts in their preexisting habits, discourses, and representations in reaction to what Funtowicz and Ravetz [1993] call post-normal science (PNS).
PNS is defined by four features, all of which apply to the COVID-19 context [Funtowicz & Ravetz, 2020]: high levels of scientific uncertainty, science policy considerations that involve values (not just evidence), high relevance to society, and an urgent need for political decision-making. Such contexts challenge the norms of science, pushing individuals to consider and engage with an “extended peer community” that includes policymakers, journalists, and members of the public. Scholars have built on this concept to propose that PNS contexts also challenge the norms of science communication, encouraging actors — such as physicians — to take on new roles and develop novel practices for engaging the public [Brüggemann, Lörcher & Walter, 2020].
1.1 Physicians’ use of social media
Previous studies indicate that Twitter/X is the platform of choice for physicians for purposes of professional networking and information sharing [Bautista, Zhang & Gwizdka, 2021; Elson et al., 2021]. This usage dates back to well before the pandemic. According to a 2011 survey, 87% of US physicians were then using social networks for personal purposes, with 67% using those platforms for professional purposes [Cooper et al., 2012]. Hanzel et al. [2018] estimated a steady growth in tweets by medical professionals since the creation of the platform in 2006, with a 95% increase in content between 2008 and 2009. Between 2016–2020, the number of physicians on Twitter more than doubled [Nakagawa, Yang, Wilson & Yellowlees, 2022].
Although physicians’ use of social media is well-established, most of the existing research focuses on their communication with peers and colleagues, rather than the public. A recent systematic review of studies published between 2006 and 2020 found that health professionals (including physicians and researchers) use social media for three primary purposes: health-related research, professional development, and doctor-patient communication [Chen & Wang, 2021]. Of the 544 studies analyzed, only one [Benetoli, Chen, Schaefer, Chaar & Aslani, 2017] provided insight into health professionals’ use of social media for public communication. That study focused specifically on pharmacists and found that participants “occasionally” used social media to provide health information and advice and “more commonly” used it to debunk health misinformation. No studies in the review investigated how doctors use social media to foster dialogues around science and health, even if encouraging such open communication with patients is part of the role of healthcare providers. However, this may have shifted during the pandemic, as physicians realized and harnessed the value of social media to not only educate patients but also engage them and advocate for them [Connell, Weyand & Barnes, 2022; Topf & Williams, 2021; Maggio, Céspedes, Fleerackers & Royan, 2024]. Moreover, physicians were called to utilize social media and even “go viral” in tackling COVID-19 related fake news [O’Connor & Murphy, 2020].
While these calls may have merit, online harassment of health professionals may keep them from maintaining an active social media presence. Almost one in four US physicians has experienced some form of online harassment [Pendergrast et al., 2021], and over 93% of the physicians and 60% of the registered nurses interviewed by Bautista et al. [2021] identified harassment and bullying as a barrier to correcting misinformation on social media. During the pandemic, 64% of physicians reported harassment resulting from their posts about COVID-19 [Royan et al., 2023].
Therefore, while there seems to be a consensus that physicians and medical professionals have a role to play in informing the public and combating misinformation, the nature and scope of that responsibility is ill-defined. Should physicians act as fact-checkers and provide corrections to the falsities circulating online? Must they become proactive communicators or merely act as expert consultants to science and health journalists? Should they fill in the gaps of pre-existing deficiencies in science and health education? And have these responsibilities changed since the outbreak of the COVID-19 pandemic?
1.2 Conceptual framework: post-normal science communication
Following the outbreak of COVID-19 in 2020, the scholars behind the concept of PNS argued that we had entered a post-normal “age”, noting that the four features of PNS — i.e., high levels of scientific uncertainty, disputes about values, high societal stakes, and an urgent need for decision making — “might have indeed been designed around the COVID-19 experience” [Funtowicz & Ravetz, 2020, p. 2]. In this volatile context, they no longer saw post-normal as a label reserved for specific, contested science issues but rather as a way to capture a more general “condition of society”.
This broader post-normal condition brings a new dimension to the concept of post-normal science communication (PNSC) proposed by Brüggemann et al. [2020]. PNSC was originally conceptualized as a response to specific PNS issues, alongside a rapidly changing media environment characterized by increasing levels of polarization and heavy use of digital networks. The authors argued that such contexts can lead to “a blurring between and a renegotiation of the professional boundaries of the stakeholders involved in science communication” as well as the development of novel communication practices, roles, and norms [Brüggemann et al., 2020, p. 2].
Brüggemann et al.’s concept paper — along with other scholarship about PNSC — has largely focused on the development of such novel practices and roles concerning specific PNS issues, such as climate change [Brüggemann, 2017; Konow-Lund, Pan & Gardell, 2024]. Scholarship about PNSC is also very limited and has focused on journalists’ adaption to PNS contexts [Brüggemann, 2017; Brüggemann et al., 2020; Fleerackers, Moorhead, Maggio, Fagan & Alperin, 2022; Fleerackers, 2023; Konow-Lund et al., 2024]. This paper expands our understanding of PNSC by examining its implications for physicians (rather than journalists) as public communicators of science and health in the context of a post-normal age (rather than a specific PNS topic).
To do so, we apply Brüggemann et al.’s [2020] framework for analyzing PNSC. Empirically, we draw on interviews with 28 physicians to examine how they responded to the unique COVID-19 context with respect to each of the four features of PNS. In our discussion, we compare these responses to what would be expected of physicians in a “normal” context, discuss possible factors driving any shift in practices, and comment on the implications for both science communication scholarship and practice.
2 Methodology
We conducted a qualitative interview study of US based physicians to understand their perceptions of their use of Twitter/X during the COVID-19 pandemic and their intentions for future use. This study was guided by a constructivist epistemology, such that our team conceptualized knowledge as socially constructed from individuals’ experiences and interactions with society [Mogashoa, 2014]. The Uniformed Services University ethics board reviewed this study, including all related study procedures and materials (e.g., interview guide, recruitment emails). The study was declared exempt by the Uniformed Services University Institutional Review Board as it was deemed to present no more than a minimal risk to participants (Case # DBS.2022.427).
2.1 Participants
Between October 2022 and April 2023, we recruited physicians based in the US who regularly used social media to engage the public. We initially identified such individuals by recruiting members of IMPACT (Illinois Medical Professionals Action Collaborative Team) or AHSM (Association of Healthcare Social Media), two grassroots organizations focused on empowering clinicians to use social media to amplify trustworthy health information. Potential participants were approached via email. Interviews were scheduled with those who agreed to participate. Snowball sampling was subsequently conducted, in which participants were asked to recommend other physician colleagues who actively used social media to communicate health information [Heckathorn & Cameron, 2017]. Throughout recruitment, we discussed whether we had reached data sufficiency — i.e., whether we felt our data allowed us to meet our research aim [LaDonna, Artino & Balmer, 2021]. We reached data sufficiency after 24 participants, but continued recruitment to ensure no new insights emerged. This resulted in 28 total participants.
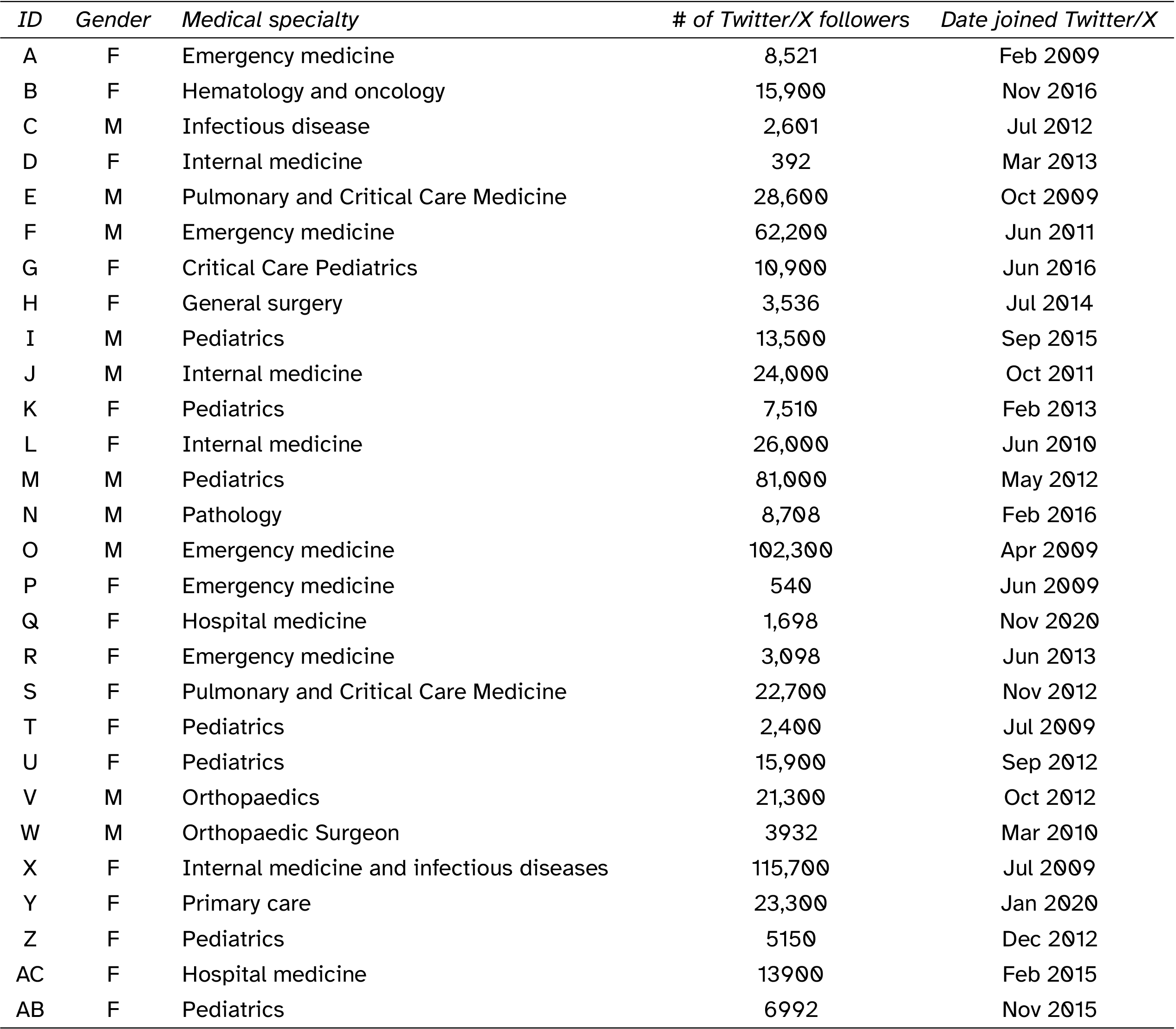
Participants were predominantly female (N = 18) and practiced at academic health centers (N = 20), which are clinical care facilities associated with schools of medicine. All participants were active Twitter users and most also engaged with additional social media platforms (e.g., Facebook, TikTok; N = 25). Participants had a range of Twitter followers ranging from 392 to 115,700 followers, with an average of 23,083 followers. Table 1 shows participants’ gender, medical specialty, number of Twitter followers,2 and date they joined Twitter.
2.2 Data collection
Data collection included interviews guided by a semi-structured interview guide (see Supplementary Materials) designed based on existing literature. The interview guide was divided into two components. The first component focused on how participants present themselves on social media and was analyzed in an earlier study [Maggio et al., 2024]. The second component focused on understanding how physicians adapted their social media use in response to COVID-19 and was influenced by Funtowicz and Ravetz’s [2020] conceptualization of PNS. Before launching the study, we piloted the interview guide with two physicians who were not included in the study sample. Based on the pilot feedback, we revised the interview guide. Throughout the study, we iterated the interview guide based on team conversations, which included reframing questions related to PNS features to better align with participants’ experiences. We also modified the interview guide in response to related world events, such as Elon Musk’s purchase of Twitter in 2022.
Interviews were conducted on Zoom or Google Meet and led by either LC or LM. On average, interviews were 40 to 60 minutes in duration. The interviews were recorded with the participant’s consent and transcribed using the platforms’ transcription features. LC and LM confirmed the accuracy of the transcripts and removed information that might identify each participant.
2.3 Analysis
We performed a reflexive thematic analysis [Braun & Clarke, 2019] of the transcripts, informed by our background and experiences. Our research team includes researchers with expertise in science and health communication (AF), science communication and sociology (LC), and health professions education and information science (LM). All authors used social media during the pandemic and followed physicians sharing health information. Our analysis was shaped by our experiences as producers, consumers, and amplifiers of social media content during a PNS “age” and in a changing social media landscape.
To become familiar with the transcripts, LC and LM closely read the complete transcripts while keeping the four features of PNS in mind. In this initial reading, they also remained open to identifying and characterizing other patterns in the data. Once familiar with the data, they met and, through discussion, agreed that the four traits of PNS were represented in the transcripts. LC and LM next independently created codes specific to PNS and applied them to a quarter of the transcripts. Codes were then compared and contrasted, and a common codebook was drafted. LC applied the codebook to all transcripts. All authors then met to reflect on and refine the resulting themes. This process allowed us to describe changes in the physicians’ online health communication practices in response to each of the core traits of PNS.
3 Results3
3.1 Facts are uncertain
Prior to the pandemic, physicians used Twitter/X in different capacities, among them, as a forum to interact with colleagues and the general public [Maggio et al., 2024]. Before the pandemic, they typically used social media to share general medical information and health recommendations — often related to their medical specialty — but this changed with the pandemic, when their content became almost completely oriented to COVID-19:
Before the pandemic I mostly posted on Twitter about medical education stuff and coronary critical care stuff. That migrated to COVID stuff during the pandemic. And now it’s become mostly health policy, frankly. (Participant E)
If you look at how people were using Twitter and what the topics were, for at least the first year or two, it was, like, dominant, right? Everyone was talking about some aspect or other of COVID policy. That includes public policy, and you know there are lots of controversial things. So yes, I’ve kind of gotten into all that, all those aspects. It did change the focus of what I tweet but that’s I think true for everybody. (Participant N)
We identified a two-fold use of social media among participants. During the first stages of the pandemic, physicians used Twitter/X as an information exchange forum to debate and share emerging information with one another about the nature of the virus, potential treatments, and methods for protecting first-line healthcare workers. As the pandemic unfolded, social media became a public-facing evidence-based information dissemination tool. Once physicians had assessed the evidence available to them, they were able to communicate it to their patients and communities:
I think initially we turned [to social media] more to find out information for ourselves and kind of how to manage these patients, how to protect ourselves — because we were recognizing that colleagues were getting sick and passed away. I think as we learned more about how the disease was getting transmitted and what we could do to contain it, then we went from, you know, “How do we manage this patient? How do we protect ourselves?” to “How can we use this platform to protect our communities?” (Participant R)
These two differentiated uses of social media are analytical; in reality, the two processes co-occurred. Navigating the scientific uncertainty of the pandemic was challenging enough for participants in their professional capacities. As public health and science communicators, this challenge doubled. The constant changes in what information could confidently be considered evidence-based produced a sense of urgency among participants, encouraging them to communicate scientific breakthroughs or policy decisions in a timely manner. Their strategies for managing uncertainty also evolved as new information became available:
With COVID, we had to learn everything in a very short period of time and during that period of time things were changing. And so our understanding was changing, not even daily but, like, by the hour sometimes. There was a lot of us learning on the fly (Participant Z).
Participants had experience communicating about health and medical science online and had handled communications involving a certain degree of uncertainty before (for example, explaining the potential of new treatments in early testing stages). However, the novelty of the coronavirus and the speed at which the disease spread around the globe exceeded the uncertainty inherent to normal science contexts. Restricted access journals and publishing houses such as Elsevier, Springer, and Wiley made their COVID-19 collections open access to make research easily available [Arrizabalaga, Otaegui, Vergara, Arrizabalaga & Méndez, 2020] as research teams worldwide reoriented their projects to study the new virus [Riccaboni & Verginer, 2022]. COVID-19-related publications and information surged. Normal science practices, such as disseminating research through scientific journal publications, were overtaken by swifter ways of sharing information, such as depositing COVID-19-related research in preprint repositories. Enabled by these changes, in the new PNS context, debates about emerging science happened in the open, on social media platforms.
The practice of sharing non-peer-reviewed papers had been commonplace among certain disciplines (notably, physics, mathematics, and astronomy) before the pandemic, but was new to many in the biomedical sciences [Puebla, Polka & Rieger, 2022]. As Participant C said: “the idea of posting things on a preprint server before the pandemic wasn’t even on my radar. We just never did that. Now we do it a lot. [ …] I think that’s most likely a permanent change”. Faced with this rapid flow of information, participants described a need to be in contact with colleagues across the globe to actively assemble and critically appraise the emerging evidence. As Participant X illustrates:
I felt like it was a firehose of information, fire hose of science, fire hose of policy, fire hose of news that you’re having to digest yourself every day. And then, how do you explain that to people in a way that’s accessible? And also make sure that you communicate that this is the best we know right now?
Participants expressed a motivation to communicate factual information about the transmission and prevention of COVID-19 as it was validated by scientists. This approach aligned with their previous, pre-pandemic uses of social media. For some physicians, debunking COVID-19-related inaccurate claims on social media developed into an extension of their medical duties, especially given reduced direct contact with regular patients and communities.
Early in the pandemic when folks weren’t able to visualize what was happening in hospitals, I felt very compelled to do that. To share things on social media and to speak up when I see things that are factually inaccurate or not what I’m seeing. I mean, if we don’t speak up, who will? The only voices that will fill that void are ones that are inaccurate. And that can definitely lead to a lot of public harm. (Participant A)
However, the practice of communicating uncertainty in a PNS context exacerbated the difficulties and challenges faced by these physicians in their function as communicators, especially when the inner mechanisms of science were exposed to the public in an accelerated manner. Practices that are part of the daily routines of scientists (e.g., testing hypotheses, replicating studies, and, most importantly, moving away from inconclusive findings, even those that initially showed promise) were revealed to the general public in real time and, in many ways, for the first time. From the perspective of participants, this brought to the fore a severe lack of public understanding of how science works — namely, that facts are often uncertain and changeable:
I think the problem during the pandemic is, the average person does not understand that science and healthcare are dynamic. They’re not static. Most of the knowledge that we have about healthcare or diseases is, you know, it’s tiny little things that we learn more very slowly over time. (Participant Z)
Physicians felt that the public’s general unfamiliarity with the internal processes of science [Millar & Wynne, 1988] created a landscape ripe for misinformation, which they attempted to combat on social media. As a result, many participants paired their COVID-specific content with posts aimed at explaining the basic processes and conditions of scientific knowledge production:
I did a lot more disclaimers because I would always say that the information is evolving and this is what we know now. [ …] so I would often say, “This is just based on the information that I have today or this may change”. I was trying very hard to make sure people understood that I was just giving them the best information I could with whatever I had at hand and that things might change. (Participant B)
One of the things that I tried to communicate is that uncertainty, being cautious in what you say, or changing what you say with information, is actually a sign of credibility, because I think that there’s this perception that if you change your position on something, it must mean that you didn’t know what you’re talking about to begin with. But actual scientific progress comes when you revise what you have to say, or learning that something that you said previously was not correct and correcting the record. That’s actually a sign of a reliable source as opposed to a reason to stop trusting them. (Participant M)
3.2 Values in dispute
While normal science is characterized by value neutrality [Funtowicz & Ravetz, 1993], in a PNS context values are disputed and play a central role in translating science into policy. For participants, the COVID-19 crisis brought to the fore historical questionings of medicine as a scientific discipline and of healthcare systems as society-serving institutions:
There’s always been some mistrust within the healthcare system because of structural racism and because of inequities and disparities that exist within medicine. And we saw that there were disparities with COVID treatment as well. [ …] Social media wasn’t going to help with that. (Participant Z)
Social media in the context of COVID-19 thus exacerbated preexisting tendencies such as mistrust in medicine, vaccine hesitancy, or suspicions around pharmaceutical companies, which led to a degradation of trust in medical expertise that was sensed by participants in their online interactions. As Participant M explained:
People seemed to be treating us nicely. I think at a certain point in the pandemic, it really did flip, and there was a switch that got shot down [ …] whatever authority we had, a lot of it got very undermined. The people to a great degree turned on that, and started rejecting it as biased.
Participants saw this bias as closely related to the polarization and politicization of scientific controversies surrounding COVID-19. Instead of the traditional neutrality of medicine and science, research and health institutions became politicized during the pandemic, as individual or collective values and political or partisan affinities shaped individuals’ acceptance or rejection of scientific discoveries and public health recommendations. Participants recognized this polarization around controversial topics such as vaccination and masking, and expressed concern about the divisiveness of certain topics. In addition, they worried about the impacts of the physicians who had similarly adopted politically charged messaging about scientific evidence: “all of a sudden you don’t necessarily know who to trust, or you can pick the physician that you want to quote because they are saying what you believe, regardless of if it’s right or wrong” (Participant P).
Participants also acknowledged that the urgency of the pandemic often resulted in changing — and even contradictory — public health guidelines, which caused the public to question political leadership and policy makers (e.g., the Centers for Disease Control [CDC], American Academy of Pediatrics). They understood and empathized with such feelings: “If it frustrated and angered me, and I’m someone that can sort of parse through some of the details, I’m sure it frustrated and angered the public understandably” (Participant T). Physicians attempted to help reduce this confusion and frustration through their social media use:
Should you wear gloves? We’re talking like April 2020, should schools stay open? What to do if your child gets sick? How to test, what did the tests mean? [ …] there was constantly changing CDC messaging on isolation and quarantine. [ …] So I made graphics. I wrote blog posts, I did a lot of that initially. (Participant U)
Public mistrust in political leadership extended to mistrust of those amplifying health recommendations. Physicians advocating for actions such as social distancing, masking, or vaccination found themselves targets of value-laden attacks from individuals who saw these guidelines as curtailing their individual freedoms or being linked to political or economic interests. Some physicians refrained from approaching controversial topics, cautious of the repercussions. At the same time, they acknowledged the difficulty of maintaining well-rounded, nuanced discussions around health policy without mentioning its social, political, or economic implications:
I think it’s really important to keep as measured responses as you can. I try really hard not to get political. Although with what’s happened recently in health care, where health care has become so political, I think that that’s become more and more difficult. (Participant B)
It definitely made me more careful about how things were going to be misread and I bet as an observer to my feed, probably made me less interesting because I was not trying to, you know, inflame anybody. (Participant J)
3.3 Stakes high
During the pandemic, stakes were high in two senses: first, in the very evident danger to the lives and health of patients, public, and physicians themselves; second, it forced physicians to grapple with new levels of online harassment. To address the first aspect of the high-stakes context, physicians’ online communication and information sharing shifted from a platform for public health education and professional or academic development to a strategy for both self-preservation and community well-being:
I’m a hospitalist. The hospitalists and ICU doctors were the very frontline physicians. We were the ones taking care of the COVID patients. [ …] We were getting extremely overwhelmed very quickly. We just felt like it was very important to try to get accurate information out as we learned it, to try to get people to protect themselves and do the right things, so that the hospitals wouldn’t get overwhelmed but also so people don’t have to go to the hospital and, you know, reduce hospitalizations, reduce deaths (Participant Q).
Simultaneously, physicians modified their approach to social media in response to growing levels of online harassment. Participants reported a heightened awareness of the consequences a tweet could trigger, as well as a more reflective attitude towards the logics of Twitter/X in particular and social media in general, both for them individually and for society as a whole. Furthermore, participants reported changing their content or tone, or refraining from commenting on certain issues, in almost a form of self censorship derived from the anticipation of aggressive responses online. In some cases, participants considered disengaging from social media entirely:
I question whether I should continue this all the time. [ …] somebody misinterprets something that I say, or I misinterpret someone else’s actions and they respond to them and I get a negative sort of feedback on that, that will completely ruin my day. [ …] I wrestle with this all the time, if I’m honest. (Participant E)
You put yourself at stake for getting personal attacks from people to talk about you, questioning your values, questioning your incentives, questioning your integrity. [ …] I don’t know if the way I use it changed, kind of the way I thought about it changed. And it made me a lot more conscious of what are the benefits about what I’m about to post, or what am I doing. (Participant W, emphasis added)
Participants also recognized the gendered, racialized component of such attacks. While almost all participants reported dealing with negative responses online, the stakes were unequal: women, people of color, and those who displayed their ethnicity as part of their online persona received higher levels of aggression and direct threats, in addition to the questioning of the content they shared:
I’ve been told for years that I’m too loud for women. I talk too fast. I talked too much for a woman. I have too many opinions. I ask too many questions. Uh, and those same qualities, you know, what’s the difference between assertive and aggressive? The answer is a Y chromosome, you know, so I will always be judged. (Participant S)
We know from the data that women and people of color are more likely to be harassed on social media. [ …] my family is originally from India and it would be things like, “elephant driver”, “go back to your country”, you know, that kind of thing, and then the C word is a favorite. “I’m going to rape you and kill you” is another favorite one. It’s not very original but it’s one that gets repeated a lot. I mean, those are things you don’t say to a man, right? And you don’t say that to a white person. (Participant X)
3.4 Decisions urgent
Under PNS, decisions are so pressing that they must be made on the basis of uncertain inputs [Funtowicz & Ravetz, 1993]. The uncertain nature of this rapidly evolving science complicated their work as both physicians and communicators, as it made it difficult to determine what information to trust and, in turn, what to translate into practice and share with their followers. In other words, participants grappled with this urgency in both their professional practice (e.g., deciding how to treat patients) and as public communicators (e.g., deciding what evidence to share and when). This sense of urgency spurred many into taking an active role in disseminating the newest available information related to COVID-19:
Uniting to combat misinformation, disinformation was important too and I did feel a responsibility during that time to promote accurate information as much as possible. I don’t know if I would have thought that same urge if I hadn’t already been involved in social media, but I did feel that way at the time and still do. (Participant G)
With the pandemic, there was a sense of urgency of communication that led me to be a lot more active on social media and also using it more for more of an advocacy role. (Participant R)
Since time was of the essence, physicians devised and deployed communication strategies to maximize the impact of their social media activity. For example, joining forces with other health professionals to amplify each others’ messages became a common practice. While these colleague-to-colleague networks had previously been informal interactions oriented to professional development, or advocacy groups around social topics beyond health and medicine (e.g., gun control or climate change activism), during the pandemic they re-oriented towards centralizing, systematizing, and sharing curated information and recommendations. Some groups even became formalized as health communication and advocacy institutions:
We created IMPACT specifically because we knew that — it didn’t seem like there was any sort of national plan coming for educating people on how to manage the pandemic or the messaging that was coming down was really inaccurate. [ …] As we went through the pandemic, we realized our infographics and our initiatives were actually really useful. We had patients who were reaching out, people in the community reaching out, saying that they really relied on our data and our stats and they relied on us quite a bit. I think that we realized how impactful our work was throughout the pandemic. (Participant B)
Participants also needed to make urgent, day-to-day decisions on how to engage with social media and, in particular, with ill-intentioned feedback, as discussed earlier. Amidst the high intensity and fast pace of communications related to COVID-19, physicians developed a more acute awareness of what could be expected after posting about certain topics or using certain language. Decisions in this line included moving away from COVID-19 content, cutting back on the time and effort spent on social media, or disengaging from social media altogether to preserve mental and emotional wellbeing, particularly once the peak of the pandemic and the initial sense of urgency had subsided:
Now we’re, what, year three in the pandemic, and I feel tired. So I’m doing it less than I was before. But I was on social media an unhealthy amount at the beginning of the pandemic for sure. (Participant B)
I don’t feel like I have the energy to do daily COVID content anymore like I used to [ …] It’s often just saying the same thing over and over again. So I am taking somewhat of a step back from that, but still going back to what I originally wanted to do, which is educate people about my specialty, educate about general medical education. (Participant I)
I guess it’s just heightened my awareness, or brought home the lesson about what social media can do and what it can’t do, and the limits of what I’m able to say, the limits of what I’m able to meaningfully engage with. (Participant M)
4 Discussion
The COVID-19 pandemic marked the start of what Funtowicz and Ravetz [2020] have called a “post-normal age”: a time characterized by extreme levels of scientific uncertainty, value-laden controversies, high societal and personal stakes, and an urgent need to make decisions to protect our collective wellbeing. These four conditions of post-normal science (PNS), defined more than two decades ago [Funtowicz & Ravetz, 1993], took place against a backdrop of an increasingly politicized and networked digital media environment, setting the stage for the established norms and practices of science communication to expand and blur [Brüggemann et al., 2020].
This study examined how this volatile communication context shaped US physicians’ use of Twitter/X to communicate science, attending to how the four features of PNS impacted their motivations and practices. We have described three major shifts: in content, in motivation, and in activity. First, physicians who used social media for general health education or to share specific content related to their medical specialty (e.g., surgery, pediatrics) turned to posting about COVID-19 almost exclusively. Because physicians had to assess, process, and publicly communicate new information almost in real time, they adopted a more critical appraisal of their sources, particularly in the face of the proliferation of non peer-reviewed research articles (i.e., preprints). The content they created and shared was specific to COVID-19, alongside broader reflections on the conditions of production of scientific knowledge, in the hopes of increasing the public’s scientific literacy.
Second, combating misinformation became one of physicians’ prime motives for engaging in social media. Many described moving from a confrontational approach — where they would openly engage and correct other Twitter users who were sharing unverified claims about COVID-19 (even fellow medical doctors and other health professionals) — to strategies more focused on amplifying reliable content so as to “drown out” misinformation. In this sense, participants perceived risks and benefits of participating in an “extended peer community” [Funtowicz & Ravetz, 1993] in discussions and decision-making processes during the pandemic. While social media exacerbated the negative consequences of the free flow of unchecked information, it also served as a forum for community engagement and acknowledgment of patients’ concerns, fears, and feelings.
Finally, whereas physicians have historically used social media to engage with one another [Bautista et al., 2021; Chen & Wang, 2021; Elson et al., 2021], our results show that during COVID-19 they became active public science communicators, drawing on their expertise to share up-to-date, accurate health and science information, debunk myths and misinformation, inform public and public health decision making, and educate audiences about what Millar and Wynne [1988] call the “internal processes of science”. As social media acted as an extension of their daily dialogues with patients [Maggio et al., 2024], physicians grappled with some of the most challenging aspects of science communication, including communicating scientific uncertainty without losing trust [Gustafson & Rice, 2020], engaging with highly contested and politicized topics [Priest, 2018], and determining the most ethical time to share emerging scientific findings [Medvecky & Leach, 2019].
Physicians’ willingness to engage the public, despite these formidable challenges, may be seen as a positive shift introduced by the pandemic. Yet at the same time, the PNS age ushered in by COVID-19 also introduced more sinister changes. In a context where “literally everything” (Participant U) was at stake, physicians deployed strategies for self-preservation. We identified shifts in their social media habits, with peaks of high intensity followed by burnout. Faced with harassment and aggression, they became more discerning in what they chose to share and how they framed it. Some took greater care when discussing controversial and politicized topics, while others began completely avoiding these issues. Still, others debated abandoning their public social media outreach entirely, especially as the urgency of the pandemic waned. Alarmingly, most participants expected these shifts in their social media use to continue. Moreover, the pressure to self-censor was highest among participants from marginalized identities — women, people of color, individuals of certain faiths — who faced the greatest levels of online harassment [Eslen-Ziya, Giorgi & Ahi, 2024]. This finding is among the most concerning identified in this study, given ongoing calls for more diverse and inclusive science communication [Canfield et al., 2020; Riedlinger, 2024; Valdez-Ward et al., 2024].
These findings must be considered alongside several limitations. Participants were exclusively US-based and English speakers. We used a non-representative sampling approach, where we recruited only physicians actively engaged in communicating about COVID-19 science and with an interest in dispelling misinformation. It should also be noted that Twitter/X is a very different digital environment today than it was when we designed and conducted the study. While not the focus of the interviews, some participants referred to their perception of an increasingly hostile online environment in the platform, which they attributed to the removal of some of the reporting mechanisms Twitter had in place prior to 2022. Moreover, the results would likely look different if we had interviewed physicians at a different point in the pandemic and would likely look even more different today. Hence, our research provides a snapshot of a particular moment in time. More research is needed to understand, on the one hand, the impacts of the communication strategies we identified on physicians’ audiences, and, on the other, the effects of the changes introduced in Twitter/X in the last two years on science and health communicators. Future research can complement this study by examining physicians’ use of social media in different geographic, cultural, and linguistic contexts, at different timepoints, on different platforms (see, for example, Atef et al.’s [2023] study on Egyptian “physician vloggers” on YouTube), and in response to different PNS situations. Finally, future studies could aim to better understand the role of organizations and networks in supporting health and science communicators in communicating about contested or polarizing topics on social media.
5 Conclusions
Originally conceptualized in the early 1990s, the applicability and explanatory power of the PNS framework was never more evident than during the COVID-19 pandemic [Funtowicz & Ravetz, 2020]. If the four core features of PNS — facts uncertain, values in dispute, stakes high, and decisions urgent — characterize changes to the conditions of production, circulation, and application of scientific knowledge, science and health communication can also change accordingly [Brüggemann et al., 2020]. In our study, we identified transformations in physicians’ communication practices, attitudes, and dispositions towards social media that can be attributed to the PNS context.
Our study makes several important scholarly contributions. Empirically, it sheds light on physicians’ use of social media during a post-normal context, an important topic which, to our knowledge, has been insufficiently studied. Theoretically, it extends the scope of the PNS communication framework [Brüggemann et al., 2020] by applying it to a new context, physicians’ use of social media during COVID-19. It further demonstrates how the four dimensions of PNS can be used as a guiding analytical frame, providing a structured approach for investigating, synthesizing, and communicating about changing science communication practices, norms, and values.
On a practical level, this study provides insights into common challenges for communicating science during PNS contexts, as well as strategies that could be used to overcome them. Ensuring communicators represent the diversity within the public is particularly pressing in the aftermath of COVID-19, as marginalized individuals and communities were disproportionately affected by the virus but may have distrusted communication from medical institutions and healthcare professionals due to long-standing inequities and mistreatment [Marcelin et al., 2021]. Moreover, the hesitancy among physicians introduced by the politicized and unsafe COVID-19 information environment has implications for their future public engagement. While every context is different, we underscore the importance of pre-existing and newly created groups and networks of physicians for developing educational material, amplifying messages, circulating trustworthy information (and collectively assessing that trustworthiness), sharing experiences, and providing emotional support to each other. Supporting such networks is essential for informing health communication strategies and policies should a new regional or global health crisis emerge in the future.
References
-
Argote, P., Barham, E., Daly, S. Z., Gerez, J. E., Marshall, J. & Pocasangre, O. (2021). The shot, the message, and the messenger: COVID-19 vaccine acceptance in Latin America. npj Vaccines 6 (1), 118. doi:10.1038/s41541-021-00380-x
-
Arrizabalaga, O., Otaegui, D., Vergara, I., Arrizabalaga, J. & Méndez, E. (2020). Open Access of COVID-19-related publications in the first quarter of 2020: a preliminary study based in PubMed. F1000Research 9, 649. doi:10.12688/f1000research.24136.2
-
Atef, N., Fleerackers, A. & Alperin, J. P. (2023). Why do health professionals create content on social media? Uses and gratifications of Egyptian “physician vloggers” on YouTube. The Journal of Social Media in Society 12 (2), 188–210. Retrieved from https://thejsms.org/index.php/JSMS/article/view/1287
-
Bautista, J. R., Zhang, Y. & Gwizdka, J. (2021). US physicians’ and nurses’ motivations, barriers, and recommendations for correcting health misinformation on social media: qualitative interview study. JMIR Public Health and Surveillance 7 (9), e27715. doi:10.2196/27715
-
Benetoli, A., Chen, T. F., Schaefer, M., Chaar, B. & Aslani, P. (2017). Do pharmacists use social media for patient care? International Journal of Clinical Pharmacy 39 (2), 364–372. doi:10.1007/s11096-017-0444-4
-
Braun, V. & Clarke, V. (2019). Reflecting on reflexive thematic analysis. Qualitative Research in Sport, Exercise and Health 11 (4), 589–597. doi:10.1080/2159676x.2019.1628806
-
Brüggemann, M. (2017). Post-normal journalism: climate journalism and its changing contribution to an unsustainable debate. In P. Berglez, U. Olausson & M. Ots (Eds.), What is sustainable journalism? Integrating the environmental, social, and economic challenges of journalism (pp. 57–73). doi:10.3726/b11462
-
Brüggemann, M., Lörcher, I. & Walter, S. (2020). Post-normal science communication: exploring the blurring boundaries of science and journalism. JCOM 19 (03), A02. doi:10.22323/2.19030202
-
Canfield, K. N., Menezes, S., Matsuda, S. B., Moore, A., Mosley Austin, A. N., Dewsbury, B. M., … Taylor, C. (2020). Science communication demands a critical approach that centers inclusion, equity, and intersectionality. Frontiers in Communication 5, 2. doi:10.3389/fcomm.2020.00002
-
Chen, J. & Wang, Y. (2021). Social media use for health purposes: systematic review. Journal of Medical Internet Research 23 (5), e17917. doi:10.2196/17917
-
Chou, W.-Y. S., Oh, A. & Klein, W. M. P. (2018). Addressing health-related misinformation on social media. JAMA 320 (23), 2417–2418. doi:10.1001/jama.2018.16865
-
Connell, N. T., Weyand, A. C. & Barnes, G. D. (2022). Use of social media in the practice of medicine. The American Journal of Medicine 135 (2), 138–140. doi:10.1016/j.amjmed.2021.08.030
-
Cooper, C. P., Gelb, C. A., Rim, S. H., Hawkins, N. A., Rodriguez, J. L. & Polonec, L. (2012). Physicians who use social media and other internet-based communication technologies. Journal of the American Medical Informatics Association 19 (6), 960–964. doi:10.1136/amiajnl-2011-000628
-
Elson, N. C., Le, D. T., Johnson, M. D., Reyna, C., Shaughnessy, E. A., Goodman, M. D. & Lewis, J. D. (2021). Characteristics of general surgery social media influencers on Twitter. The American Surgeon 87 (3), 492–498. doi:10.1177/0003134820951427
-
Eslen-Ziya, H., Giorgi, A. & Ahi, C. J. (2024). Digital vulnerabilities and online harassment of academics, consequences, and coping strategies: an exploratory analysis. Feminist Media Studies 24 (6), 1422–1427. doi:10.1080/14680777.2023.2281268
-
Fleerackers, A. (2023). Unreviewed science in the news: why and how journalists cover preprint research (Ph.D. Thesis, Simon Fraser University). Retrieved from https://summit.sfu.ca/item/36680
-
Fleerackers, A., Moorhead, L. L., Maggio, L. A., Fagan, K. & Alperin, J. P. (2022). Science in motion: a qualitative analysis of journalists’ use and perception of preprints. PLoS ONE 17 (11), e0277769. doi:10.1371/journal.pone.0277769
-
Funtowicz, S. O. & Ravetz, J. R. (1993). Science for the post-normal age. Futures 25 (7), 739–755. doi:10.1016/0016-3287(93)90022-L
-
Funtowicz, S. O. & Ravetz, J. R. (2020). Science for the post-normal age. Commonplace. doi:10.21428/6ffd8432.8a99dd09
-
Gustafson, A. & Rice, R. E. (2020). A review of the effects of uncertainty in public science communication. Public Understanding of Science 29 (6), 614–633. doi:10.1177/0963662520942122
-
Hanzel, T., Richards, J., Schwitters, P., Smith, K., Wendland, K., Martin, J. & Keltgen, J. (2018). #DocsOnTwitter: how physicians use social media to build social capital. Hospital Topics 96 (1), 9–17. doi:10.1080/00185868.2017.1354558
-
Heckathorn, D. D. & Cameron, C. J. (2017). Network sampling: from snowball and multiplicity to respondent-driven sampling. Annual Review of Sociology 43 (1), 101–119. doi:10.1146/annurev-soc-060116-053556
-
Konow-Lund, M., Pan, L. & Gardell, E.-K. O. (2024). How COVID-19 affected the practice of investigative journalism in Norway and China. In M. Konow-Lund, M. Park & S. Bebawi (Eds.), Hybrid investigative journalism (pp. 137–165). doi:10.1007/978-3-031-41939-3_9
-
LaDonna, K. A., Artino, A. R. & Balmer, D. F. (2021). Beyond the guise of saturation: rigor and qualitative interview data. Journal of Graduate Medical Education 13 (5), 607–611. doi:10.4300/jgme-d-21-00752.1
-
Maggio, L. A., Céspedes, L., Fleerackers, A. & Royan, R. (2024). ‘My doctor self and my human self’: a qualitative study of physicians’ presentation of self on social media. Medical Education 58 (10), 1192–1204. doi:10.1111/medu.15384
-
Marcelin, J. R., Swartz, T. H., Bernice, F., Berthaud, V., Christian, R., da Costa, C., … Abdul-Mutakabbir, J. C. (2021). Addressing and inspiring vaccine confidence in Black, Indigenous, and People of Color during the coronavirus disease 2019 pandemic. Open Forum Infectious Diseases 8 (9), ofab417. doi:10.1093/ofid/ofab417
-
Medvecky, F. & Leach, J. (2019). An ethics of science communication. Springer International Publishing. doi:10.1007/978-3-030-32116-1
-
Millar, R. & Wynne, B. (1988). Public understanding of science: from contents to processes. International Journal of Science Education 10 (4), 388–398. doi:10.1080/0950069880100406
-
Mogashoa, T. (2014). Applicability of constructivist theory in qualitative educational research. American International Journal of Contemporary Research 4 (7), 51–59. Retrieved from http://www.aijcrnet.com/journal/index/758
-
Nakagawa, K., Yang, N. T., Wilson, M. & Yellowlees, P. (2022). Twitter usage among physicians from 2016 to 2020: algorithm development and longitudinal analysis study. Journal of Medical Internet Research 24 (9), e37752. doi:10.2196/37752
-
O’Connor, C. & Murphy, M. (2020). Going viral: doctors must tackle fake news in the covid-19 pandemic. BMJ 369, m1587. doi:10.1136/bmj.m1587
-
Office of the Surgeon General (2021). Protecting youth mental health: the U.S. Surgeon General’s advisory. Washington, DC, U.S.A.: US Department of Health and Human Services. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK575984/
-
Pan American Health Organization (2020). Understanding the infodemic and misinformation in the fight against COVID-19. Retrieved from https://iris.paho.org/bitstream/handle/10665.2/52052/Factsheet-infodemic_eng.pdf
-
Pendergrast, T. R., Jain, S., Trueger, N. S., Gottlieb, M., Woitowich, N. C. & Arora, V. M. (2021). Prevalence of personal attacks and sexual harassment of physicians on social media. JAMA Internal Medicine 181 (4), 550–552. doi:10.1001/jamainternmed.2020.7235
-
Priest, S. (2018). Communicating climate change and other evidence-based controversies: challenges to ethics and practice. In S. Priest, J. Goodwin & M. F. Dahlstrom (Eds.), Ethics and practice in science communication (pp. 55–72). Chicago, IL, U.S.A.: University of Chicago Press.
-
Puebla, I., Polka, J. & Rieger, O. Y. (2022). Preprints: their evolving role in science communication. Ann Arbor, MI, U.S.A.: Against the Grain (Media), LLC. doi:10.3998/mpub.12412508
-
Riccaboni, M. & Verginer, L. (2022). The impact of the COVID-19 pandemic on scientific research in the life sciences. PLoS ONE 17 (2), e0263001. doi:10.1371/journal.pone.0263001
-
Riedlinger, M. (2024). Welcome to 2024: issues and trends occupying JCOM this year. JCOM 23 (01), E. doi:10.22323/2.23010501
-
Royan, R., Pendergrast, T. R., Del Rios, M., Rotolo, S. M., Trueger, N. S., Bloomgarden, E., … Arora, V. M. (2022). Use of Twitter amplifiers by medical professionals to combat misinformation during the COVID-19 pandemic. Journal of Medical Internet Research 24 (7), e38324. doi:10.2196/38324
-
Royan, R., Pendergrast, T. R., Woitowich, N. C., Trueger, N. S., Wooten, L., Jain, S. & Arora, V. M. (2023). Physician and biomedical scientist harassment on social media during the COVID-19 pandemic. JAMA Network Open 6 (6), e2318315. doi:10.1001/jamanetworkopen.2023.18315
-
Sallam, M. (2021). COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines 9 (2), 160. doi:10.3390/vaccines9020160
-
Southwell, B. G., Brennen, J. S. B., Paquin, R., Boudewyns, V. & Zeng, J. (2022). Defining and measuring scientific misinformation. The ANNALS of the American Academy of Political and Social Science 700 (1), 98–111. doi:10.1177/00027162221084709
-
Southwell, B. G., Thorson, E. A. & Sheble, L. (2017). The persistence and peril of misinformation. American Scientist 105 (6), 372. doi:10.1511/2017.105.6.372
-
Suran, M. & Bucher, K. (2024). False health claims abound, but physicians are still the most trusted source for health information. JAMA 331 (19), 1612–1613. doi:10.1001/jama.2024.6837
-
Tangcharoensathien, V., Calleja, N., Nguyen, T., Purnat, T., D’Agostino, M., Garcia-Saiso, S., … Briand, S. (2020). Framework for managing the COVID-19 infodemic: methods and results of an online, crowdsourced WHO technical consultation. Journal of Medical Internet Research 22 (6), e19659. doi:10.2196/19659
-
ThisIsOurShot (n.d.). About us. Retrieved August 16, 2024, from https://thisisourshot.info/about-us/
-
Thompson, T. L., Parrott, R. & Nussbaum, J. F. (Eds.) (2011). The Routledge handbook of health communication (2nd ed.). New York, NY, U.S.A.: Routledge. doi:10.4324/9780203846063
-
Those Nerdy Girls (2022). Dear pandemic: empowering women to navigate the flood of information. World Health Organization Information Network for Epidemics. Retrieved from https://cdn.who.int/media/docs/default-source/science-translation/case-studies-1/cs10_dearpandemic.pdf
-
Topf, J. M. & Williams, P. N. (2021). COVID-19, social media, and the role of the public physician. Blood Purification 50 (4–5), 595–601. doi:10.1159/000512707
-
Valdez-Ward, E., Ulrich, R. N., Bennett, N., Martinez-Maldonado, E., Mattheis, A., Treseder, K. K., … Menezes, S. (2024). Science communicators from marginalized backgrounds challenge STEM cultural norms to promote community belonging. JCOM 23 (04), A01. doi:10.22323/2.23040201
-
Zarocostas, J. (2020). How to fight an infodemic. The Lancet 395 (10225), 676. doi:10.1016/S0140-6736(20)30461-X
Notes
1. While misinformation can be created and shared unintentionally, disinformation implies a deliberate purpose or intention from the sender to deceive or alienate the recipient. Both phenomena are concerning; however, in this paper we focus on misinformation in the context of the COVID-19 pandemic, adhering to Southwell et al.’s [2017] perspective that considers disinformation “as a special type of misinformation distinguished by the promoter’s intent” and acknowledges that “false information can mislead people even if unintentionally promoted or mistakenly endorsed as the truth”.
2. As of the date of recruitment for this study. Follower counts may have increased or decreased since then.
3. For further participant quotes, see the tables in the Supplementary material.
About the authors
Lucía Céspedes (she/her) is member of the UNESCO Chair in Open Science and a research counselor at the Consortium Érudit, Université de Montréal, Canada. She is also research assistant at the Scholarly Communications Lab at Simon Fraser University. Her research brings together sociolinguistics, social studies of science and technology, and scholarly communication, in order to analyze conditions of production and circulation of scientific knowledge in centres and peripheries.
E-mail: lucia.cespedes@umontreal.ca X: @c_est_lucy
Alice Fleerackers (she/her) is a postdoctoral research fellow at the University of British Columbia’s School of Journalism, Writing, and Media and the Scholarly Communications Lab at Simon Fraser University. She studies the intersections of health and science communication, journalism, digital media, equity, and open science. She is also a freelance science writer and the co-founder and co-chair of the Diversity, Equity, Inclusion, and Accessibility Committee of the Public Communication of Science and Technology Network. Find her at alicefleerackers.com.
E-mail: afleerac@mail.ubc.ca X: @FleerackersA
Lauren A. Maggio is a Professor of Medical Education at the University of Illinois Chicago. Her research explores the creation, dissemination and use of biomedical information. In particular, she examines how to effectively connect physicians, learners, and patients with biomedical information through the design of educational interventions and technical solutions, and by facilitating access to knowledge for public and professional use. Dr. Maggio also explores and advocates for the responsible conduct of research, including practices related to authorship.
E-mail: lmaggio@uic.edu X: @Lauren_Maggio
Supplementary material
Available at https://doi.org/10.22323/2.23060204
Interview Guide
Table A: Representative participant quotations related to the four traits of post normal
science
Table B: Representative participant quotations regarding normal vs. post-normal science
communication practices